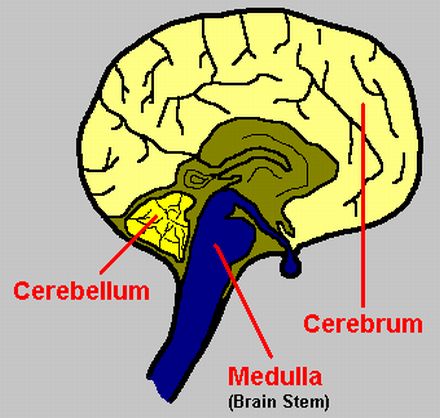
The second most common region for multiple sclerosis attacks is the brain stem-cerebellar area, making up approximately 38% of all relapses. There is a term called “Charcot’s Triad”, named after neurologist Jean-Martin Charcot, which describes the most prevalent symptoms resulting from these attacks: speech difficulties, compromised balance, and double vision. Brain stem-cerebellar attacks can cause any of the following symptoms in an MS patient:
Loss of Balance and Coordination
These problems can involve walking, rising to a standing position, using the legs, and/or using the arms and hands. MSers can have difficulties with walking and may sway to one side, or possibly experience vertigo or dizziness (along with nausea.) Loss of coordination, also referred to as ataxia, can affect the fine movements of the hands and make writing, combing one’s hair, and tying shoe laces very difficult. Another manifestation of this damage is an intention tremor, where the hand or hands shake. Patients also describe problems with clumsiness and the coordination of limbs.
Eye and Vision Abnormalities
There are two types of eye problems associated with brain stem and cerebellar attacks. The first is eye muscle jerking, or nystagmus, which causes vision to be “jumpy'” or moving. The second type is eye muscle weakness, or gaze palsy, which can cause double vision.
Speech and Swallowing Disturbances
Problems with speech, also known as dysarthria, can affect the rhythm or pronunciation of words. The slurring of words is one disorder, where a person might appear to be intoxicated. Rhythm can be affected too, and a patient may find herself “scanning” or speaking in a jerky or stuttering fashion. Problems with swallowing, or dysphagia, may also occur.
Trouble with Facial Muscles and Nerves
Weakness, muscle spasms, numbness, and pain may occur in facial muscles. A particular facial nerve that may be affected is the trigeminal nerve, which runs along both sides of the face. This can cause severe pain blasts or dull, achy pain along the cheeks and jawlines.
Tinnitus (Ear Pain and Ringing)
This is a less common problem. In severe cases, a loss of hearing may result. This is generally limited to one ear.
Emotional Disturbances
Inappropriate laughing, crying (emotional lability), and euphoria (exaggerated sense of wellbeing) can be noted with brain stem and cerebellar attacks. These symptoms are considered separate from multiple sclerosis depression, which appears to originate from damage to the cerebrum.
Reference:
Rosner, Louis J., MD and Shelley Ross. Multiple Sclerosis: New Hope and Practical Advice for People with MS and their Families. Simon & Schuster: New York, NY, 2008.

